
Dear readers!
The book “Hemangioma” is written for medical students, doctors of various specialties who encounter this disease in their practice, as well as for interested parents of young patients. This book is not a guide to self-treatment and self-diagnosis. The book talks about modern approaches and views on this pathology and emphasizes that infant hemangiomas are a serious problem of the present time. Considering the complexity of this disease, infant hemangiomas should be treated with due attention and professionalism.
Important: treatment can only be prescribed by a doctor!*
Author

Director and founder of the “Center for Vascular Pathology” (Moscow) clinic, pediatric surgeon, laser treatment specialist, interventional radiologist.
Specialist advice is required.
Contents
Preface
Infantile hemangiomas have become a very common pathology in recent years, with almost every hundredth infant suffering from this disease. And if just 5−7 years ago the problem of diagnosis and treatment was extremely urgent, now many specialists are able not only to correctly diagnose, but also to perform the necessary treatment. But, unfortunately, there are not enough such specialists yet. Our Center for Vascular Pathology is the leading clinic in Russia for the treatment of vascular pathology in children and adults. This book contains and updates the main questions that arise not only among specialists, but also among any medical doctors who encounter this pathology. The book reflects modern views on the medical aspects of this problem. My personal experience of working with patients with vascular pathology since 2011, the experience of my colleagues and our Center for Vascular Pathology are reflected in this publication.
In working on this publication I was assisted by: Bryleeva Anastasia Aleksandrovna, Rakhimov Amriddin Ravshanovich, Denisevich Svetlana Sergeevna.
I express my deep gratitude to Postevaya Alina Anatolyevna for preparing and editing the material for the book.
April 12, 2022
Dmitry V. Romanov
There are no manuals in Russian medical literature that would cover the problem of treating vascular tumors in sufficient detail. Individual chapters and small sections of general manuals are clearly insufficient for a practicing physician, and articles scattered across the pages of periodicals, usually treating one of the many methods of treatment, are unable to give the reader an idea of all aspects of the problem. Thus, the latter is deprived of the opportunity to compare and choose one or another method in each specific case.
S.A. Kholdin
“Hemangiomas and their treatment”
1935
Introduction
1. What is an infantile hemangioma?
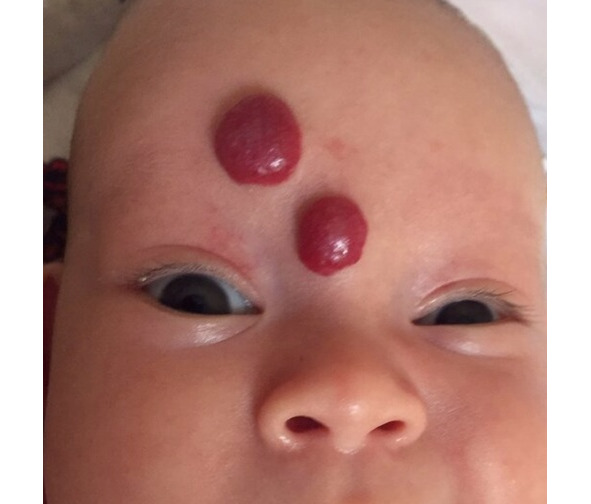
Infantile hemangioma is a benign vascular tumor that is formed in utero and develops in the first weeks after birth. Distinctive features of the tumor are active growth in the first months of life and the ability to involution over the following years.


2. Why infantile hemangioma and not children’s hemangioma?
In English literature, hemangiomas are referred to as infantile hemangioma, the literal translation is “children’s hemangioma” or “infantile hemangioma”, but the words “children’s” and “infantile” do not reflect the essence of the disease, the disease occurs in the period of “infancy” — early childhood up to one year.
The phrase “infantile hemangioma” most fully describes the time of development and the essence of the disease, so we will use and consider it correct to use the term — “infantile hemangioma”.
3. Is hemangioma a tumor?
The term “hemangioma” (from the Greek haima — blood, angeion — vessel and -oma ending denotes the names of tumors) is a benign tumor of blood vessels. According to the classification of the International Society for the Study of Vascular Anomalies (ISSVA), infantile hemangiomas are classified as vascular tumors. The conducted immunohistochemical studies confirm the fact of the individuality of this nosological unit and the tumor-like nature of the disease.
4. Can infantile hemangioma become malignant?
Infantile hemangioma is a benign vascular tumor. It cannot become malignant over time, or with surgical, laser, or other treatments.
5. What tissue does hemangioma grow from?
Infantile hemangioma is formed embryonically from hemogenic epithelium, which, under the influence of certain factors, first develops into mesenchymal stem cells and endothelial progenitor cells, then into pericytes and endothelial cells, from which abnormal blood vessels are subsequently formed.
6. What is endothelium?
Endothelium is a single-layered sheet of flat cells of mesenchymal origin lining the inner surface of blood and lymphatic vessels, and the chambers of the heart. Endothelial cells perform many functions of the vascular system, such as: vasoconstriction and vasodilation, control of blood pressure; regulation of blood clotting components, namely thrombin and fibrin; angiogenesis (formation of new blood vessels).

7. What are pericytes?
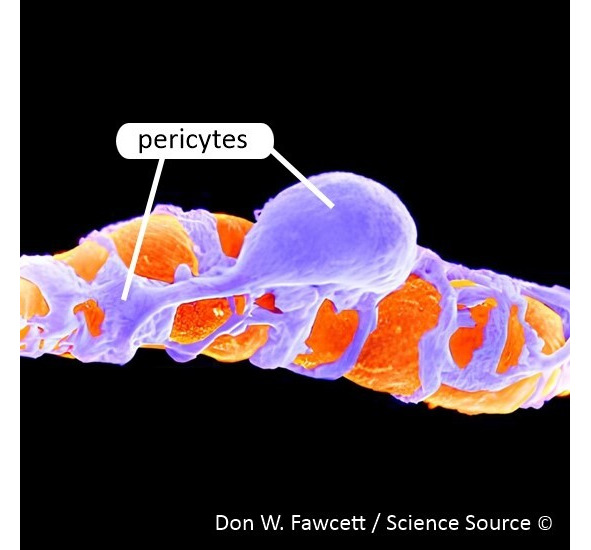
Pericyte (from the ancient Greek περι- — around, near and κύτος — cell), or Rouget cell, is a branched cell of connective tissue.
Pericytes are part of the walls of small blood vessels, including capillaries.
8. What is angiogenesis?
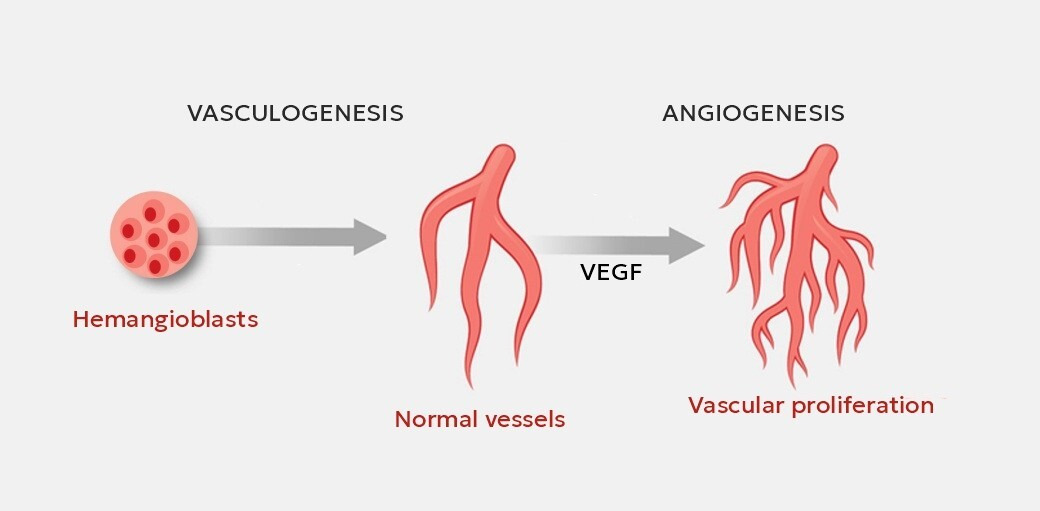
Angiogenesis is the process of formation of new blood vessels in an organ or tissue, leading to the reorganization of the primary capillary network, which is reduced to a simpler and more distinct system of capillaries, arteries and veins. Normally, angiogenesis processes in the body occur with moderate intensity and are activated only during the regeneration of damaged tissues, the formation of blood clots, the elimination of inflammation, the formation of a scar and similar recovery processes.
Vasculogenesis is the process of formation of blood vessels from endothelial progenitor cells (EPCs), which differentiate into endothelial cells, forming new vessels. This form of vessel formation is characteristic of the embryonic period, when the formation of the primary vascular plexus occurs.
I. Classification
1.1. What is the current classification of vascular anomalies?
The main working classification for specialists in the field of vascular pathology is the classification of the International Society for the Study of Vascular Anomalies (ISSVA) (Table 1). The latest changes to the Classification were made in April 2018.
In 1962, Soviet surgeons Ternovsky S.D. and Kondrashin N.I. proposed dividing vascular tumors and vascular anomalies into 2 main groups of pathological changes, and only 20 years later, in 1982, Mulliken and Glowacki proposed a similar division, confirming the assumptions of Russian researchers with immunohistochemical studies.
1.2. What is a cavernous hemangioma?
The word “cavern” comes from the Latin word “caverna” — a cave, a cavity. In medicine, caverns were defined as pathological cavities that arise in the body as a result of partial tissue necrosis followed by its decay and rejection of the dead mass. The question arises, what does hemangiomas have to do with it? The term “cavernous hemangioma” appeared in the early 19th century and implied pathologically dilated vessels in the form of cavities of various sizes and shapes. Due to the lack of any other clarifying research methods (at that time there was only microscopy and histology), this term was retained in subsequent years, was included in classifications and was used to designate a number of pathological conditions characterized by tumor-like proliferation of vessels, most of which were dilated and had vascular cavities on the section. After the advent of immunohistochemistry, this term lost its significance, as it became possible to accurately determine the tissue nature of these pathological conditions. Today, many cavernous hemangiomas turn out to be venous or arteriovenous malformations.
1.3. What is a capillary hemangioma?
The term capillary hemangioma appeared during the period of using the term “cavernous hemangioma”, based on histological studies, due to the prevalence of pathological capillaries in the tissues under study, all infantile hemangiomas at that time were considered capillary hemangiomas and in some cases continue to be considered (especially in the conclusions of pathologists). At present, this term has lost its meaning.
1.4. What are the types of hemangiomas?
Infantile hemangiomas are divided into the following types according to the prevalence of the pathological process:
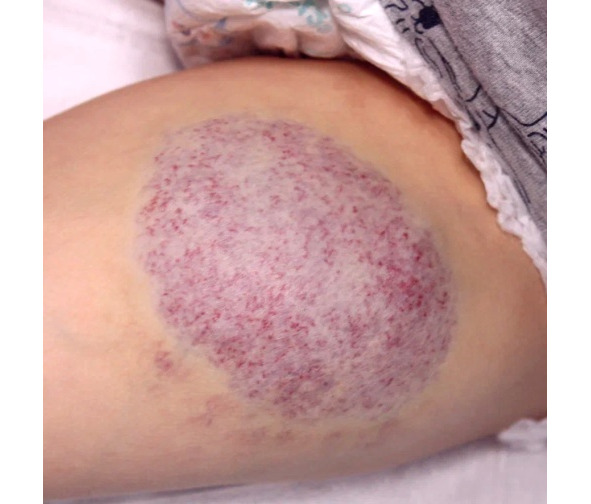
— superficial (the tumor-like formation spreads superficially and affects all layers of the dermis);
— deep (the tumor-like formation is located subcutaneously, in most cases there are no vascular manifestations on the surface of the skin, or isolated telangiectasias are observed);
— combined (a combination of superficial and deep pathological changes).



According to the area of damage, infantile hemangiomas are divided into:
— focal (damage to one anatomical area);
— multifocal (damage to several anatomically unrelated areas);
— segmental (damage to several adjacent anatomical areas at once).

1.5. What is a congenital hemangioma?
A congenital hemangioma differs from an infantile hemangioma not only in that it is laid down in utero, but also in the intrauterine onset of the development cycle and formation of pathological volumetric vascular tissue. At the time of birth, a congenital hemangioma has its maximum size; no growth of the hemangioma after birth is observed. Some specialists mistakenly classify congenital hemangiomas as infantile, assuming that they began their tumor-like development in utero, and by the time of birth they have completed the proliferation phase (active growth), but immunohistochemical and genetic studies have shown that these tumor-like formations have different natures and cannot be combined into one term “infantile hemangioma”. After birth, congenital hemangiomas can involute on their own, partially or completely, but in some cases, congenital hemangiomas remain unchanged over the following years.


1.6. What types of congenital hemangioma are there?
Congenital hemangiomas are divided into:
— rapidly involuting congenital hemangioma (RICH);
— non-involuting congenital hemangioma (NICH);
— partially involuting congenital hemangioma (PICH).
1.7. What is the difference between congenital hemangiomas?
The most similar clinical picture when examining a patient are RICH and PICH hemangiomas. It is not for nothing that 5 years ago only 2 types of congenital hemangiomas were determined RICH and NICH and only recent studies have revealed the PICH variant. The tumor-like formation does not have smooth contours and may also rise unevenly above the surface of the skin.

Hemangiomas are capable of rapid involution during the first months from the moment of birth in cases with RICH — complete disappearance with a deficit of subcutaneous fat in this place subsequently, and in the case of PICH with partial involution of pathological tissue, usually more than 50−60% of the volume.
NICH hemangiomas are characterized by the appearance of a low cylinder (like a “washer”), protruding quite evenly above the surface of the skin, dense upon palpation, on the surface of which venulo- and telangiectasias are determined; the classic variant of infantile hemangiomas — red papules — are not determined on the surface of the tumor. After birth, the tumor remains unchanged (NICH hemangioma).


All types of these hemangiomas are not sensitive to the administration of beta-blockers.
1.8. What is a segmental hemangioma?
The term “segmental lesion” came to this area of medicine from maxillofacial surgery and implies the involvement of several anatomical areas in the pathological process at once (for example, the forehead, orbit, cheek, or, for example, the hand and forearm).


When segmental hemangioma is detected in a patient, it is necessary to exclude the presence of combined pathological syndromes, such as PHACE (s) and LUMBAR.
1.9. What is hemangiomatosis?
Hemangiomatosis is the presence of multiple (more than 4−5) hemangiomas on the skin (and/or mucous membrane) of a child. The number of hemangiomas in hemangiomatosis can vary from 5 to 1000 or more elements. In our practice, the maximum number of infantile hemangiomas detected in one child was 1096 elements, and there was damage not only to the skin, but also to visible mucous membranes (lips, oral mucosa, tongue, palate). The forms and types of hemangiomas in hemangiomatosis can be variable, but as a rule, these are small tumor-like formations, mainly up to 2−3 mm in diameter.
There are two types of hemangiomatosis:
— benign neonatal hemangiomatosis (only the skin is affected);
— diffuse neonatal hemangiomatosis, in which, in addition to the skin, hemangiomas affect the parenchyma of the liver/spleen/intestine.


1.10. What internal organs can be affected by hemangioma?
Most often, pathological changes are detected in the largest parenchymatous organ of a person — in the liver. These pathological changes in a newborn are usually determined by a standard screening ultrasound examination. Detection of infantile hemangiomas of the spleen and kidneys in a newborn by ultrasound examination is extremely rare.
There are three types of liver damage by infantile hemangioma: focal (28%), multiple (57%) and diffuse (15%).
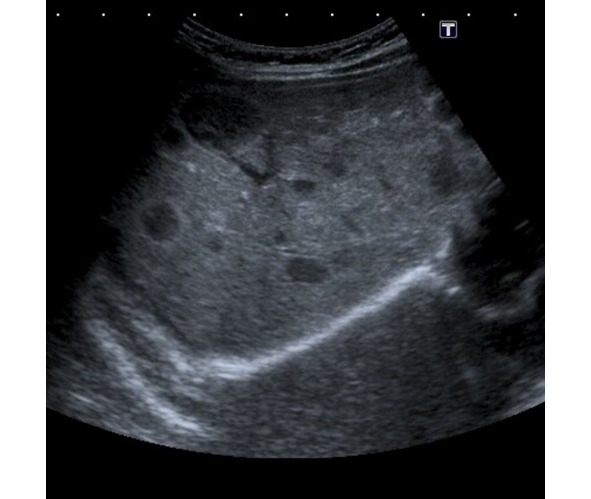

Focal hemangioma of the liver (28%) is a rapidly involuting hemangioma that regresses immediately after birth. The incidence in boys and girls is the same. About 15% of children have infantile hemangiomas on their skin. More than 90% of the tumor volume decreases by 1.5−2 years of age.
Multiple hemangioma of the liver (57%) is an infantile hemangioma that is very often accompanied by skin manifestations (77%). It is usually detected during liver screening examination in children with hemangiomatosis. This type of hemangioma occurs 2–3 times more often in girls than in boys. Since all infantile hemangiomas develop after birth, multiple hemangioma of the liver cannot be diagnosed prenatally by ultrasound examination. After involution of the infantile hemangioma of the liver, the parenchyma involved in the pathological process becomes normal.
Diffuse hemangioma of the liver (15%) is an infantile hemangioma that is very often detected during the neonatal period. Diffuse hemangioma of the liver is not represented by normal liver tissue — the entire liver is replaced by a tumor. Half of the patients have skin hemangiomas. Girls are more often affected (in 70% of cases). With this change, liver function disorders are possible — liver failure.
1.11. What is Kaposiform hemangioendothelioma (hemangioendothelioma)?
Kaposiform hemangioendothelioma is a rare vascular tumor characterized by local aggression, but without metastasis. The incidence rate is approximately 1:100,000 children. This disease has no gender, boys and girls suffer from this disease with equal frequency. The head and neck are most often affected (40%), less often the trunk (30%) or limbs (30%). In the neonatal period, it occurs in 60% of cases, and is detected in 93% of cases during infancy.
This diagnosis can also be made at an older age. Kaposiform hemangioendothelioma can occur in adults. The main method confirming the presence of Kaposiform hemangioendothelioma in a patient is an immunohistochemical study of removed pathological tissues.


71% of patients with this vascular tumor have life-threatening Kasabach-Merritt syndrome.
1.12. What is Kasabach-Merritt syndrome (phenomenon)?
Kasabach-Merritt syndrome, also known as “hemangioma syndrome with thrombocytopenia”, most often manifests itself as the presence of Kaposiform hemangioendothelioma, which is complicated by thrombocytopenia (a significant decrease in the number of platelets), hemolytic anemia (destruction of red blood cells) and coagulopathy (impaired blood clotting). All these factors lead to severe bleeding. Kasabach-Merritt syndrome occurs equally often in boys and girls.
Attempts to take histological material or perform surgery to remove hemangioendothelioma without first excluding Kasabach-Merritt syndrome lead to the development of life-threatening bleeding both during the operation and in the subsequent period!
1.13. What vascular formation is most often confused with infantile hemangioma?
The second most common vascular formation in pediatric practice is pyogenic granuloma. The primary distinguishing feature of pyogenic granuloma from infantile hemangioma is the appearance of a local round formation in children over 3 months of age.
Conventionally, the third most common and most misdiagnosed nevus is Spitz’s nevus.
1.14. What is pyogenic granuloma?
Pyogenic granuloma is also called lobular capillary hemangioma. In most cases, acquired granuloma occurs, but cases of congenital pyogenic granuloma have also been described. A feature of pyogenic granuloma is rapid (eruptive, explosive) growth. This formation develops literally in a few days. The granuloma is a dense red papule that grows quickly and has a base in the form of a stalk (leg).


Pyogenic granuloma is characterized by bleeding and ulceration. After bleeding and crust falling off, it may become smaller, but usually grows again, already with a larger base and a more dome-shaped raised part. Most often, pyogenic granuloma appears at the age of 3−7 years and only in 12% — in the first year of life. Pyogenic granuloma most often affects the skin (88.2%), less often — mucous membranes (11.8%). It occurs on the head and neck in 62% of cases, on the trunk — in 20%, on the upper limbs — in 13%, on the lower limbs — in 5%.
Patients have a history of microtraumas of the skin at the site of formation of pyogenic granuloma: cracks in the skin, allergies and dermatitis, scratching, insect bites (mosquitoes).
1.15. What is Spitz naevus?
Spitz naevus is a relatively rare benign type of skin tumor. Spitz naevus is part of a group of skin tumors commonly called moles. Spitz nevi initially grow rapidly, forming pink or brown bumps on the surface of the skin.
They are usually found on the head, neck, or legs of children and young adults. The tumor is named after Dr. Sophie Spitz, a pathologist who first described these nevi.
Бесплатный фрагмент закончился.
Купите книгу, чтобы продолжить чтение.